Getting and Giving Bad News Remotely
Telemedicine in the Time of COVID

Today’s post is not particularly journalism-y, but our fearless leader gave me the keys to the kingdom and told me I could write whatever I wanted. So, here’s some deeply personal stuff in the times of COVID.
We’ve been socially distanced in our homes in beautiful suburban Iowa for 24 days. Maybe 25 days? I don’t even know what day it is anymore. Maybe its Thwednesday, Maypril 39th? I have no idea. All of the days have blurred together. While the major focus of discussions seems to revolve around the ongoing COVID pandemic, there are still patients who need routine management of other conditions or who may have developed non-COVID related symptoms who still need treatment. I’ve been amazed at the telemedicine efforts I’ve watched unfold at my university hospital. Lots of doctors, nurses, and other care providers, dressed from the waist up, doing their best to fill the stop gaps in care that have been created by the inability to see patients in person.
I’ve recently seen oncologists talking online about how they are delivering “bad news” via telemedicine. All seem positive with discussions of whether phone or video is the best way to tell someone they have something that may kill them. For example, this thread:
I am a medical oncologist, and a frequent part of my job is giving people bad news. Due to the pandemic I have been doing almost all of my clinic visits by phone or video the past three weeks, and I have some reflections on giving bad news remotely 1/9
— Garth Nicholas (@Garth_Nicholas1) April 2, 2020
Well, to that end, I have recently received some bad news remotely and I have some reflections as well.
Receiving bad news sucks. Receiving bad news remotely in the COVID era sucks exponentially more.
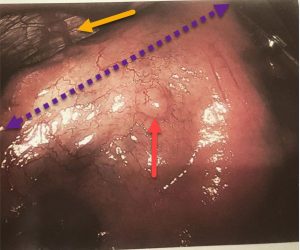
I’ve spoken on Twitter about the surgery I had almost a year ago to remove 85% of my stomach. I had a, thankfully, small gastrointestinal stromal tumor (GIST) on my stomach and GIST cancer can become a problem if left untreated. Mine had nice clear borders and was in an easily resectable place, but the last year has been a lesson in being able to keep up with my caloric needs with a 2 oz stomach. On the bright side, I had the 80 lbs I’ve lost to spare.
But, it’s kind of weird for a woman my age to have a GIST since most are found in people over 50 years old. At the time, my surgeon assured me it was likely a random thing and I shouldn’t lose sleep. I called my favorite aunt to commiserate after surgery and told her about my tumor. She replied, “Wow. That’s really weird. My grandmother died at 28 years old of ‘stomach sarcoma.’ And my dad had early colon cancer. And you know, your mom had that cervical or uterine thing. What are the odds??”
What are the odds, my friend? What are the odds, indeed. I went to one of my colleagues at our cancer center and posed the question to him. He recommended that I follow up with genetic testing to see if I had any heritable mutation that might explain my early tumor or whether me, my great grandmother, her son, and my mother, are explainable by some sort of heritable mutation. You can guess where this is going.
I had myself sequenced according to a standard, heritable cancer panel from a commercial company. Interestingly, my insurance didn’t cover my screening because I didn’t really have a definitive family pedigree. Just my aunt’s report that there might have been some early cancer in the tree and I don’t know much about anything on my dad’s side of the family. I was supposed to follow up with the genetic counselor in person for my results, but that was canceled when COVID restrictions were placed on our hospital. Instead, she called me to ask if I wanted my results by phone and then called me a few days later to actually deliver my results. It was agony to have to wait for her to call me after she had already called me.
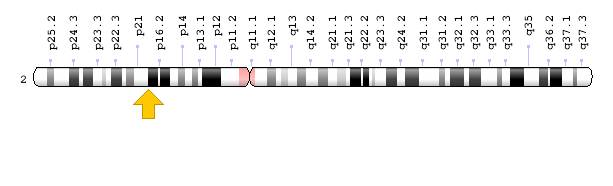
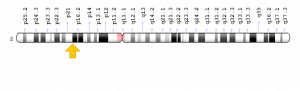
I have a heritable, pathogenic mutation in my MSH6 gene, which is responsible for DNA repair. Mutations in genes like MSH6 cause Lynch Syndrome. I’m still trying to wrap my mind around that. People with Lynch Syndrome have an 8-fold increased risk of colorectal cancer and a 26-fold increased risk of endometrial cancer. They can also develop tumors in other sites like the stomach and small bowel. It is recommended that people with Lynch Syndrome have an annual colonoscopy and women should have a prophylactic hysterectomy. I’ve already lost my stomach and I’m probably going to lose my reproductive organs as well. I also don’t really know that I am cancer free from the stomach down. I could be brewing another time bomb in my colon and my uterus. I’m still really struggling with this and I learned it in a phone call.
Before I got that call, I was discussing with Strange how telemedicine might completely change how we practice medicine. Maybe it would free up more of the hospital for other patients who really “need” the resources. Now I’m rethinking that thought exercise.
Learning about my diagnosis in-person versus over the phone would have been an entirely different experience, even though the person who delivered my news was as kind and compassionate as anyone I’ve met in healthcare. I would have had my husband sitting next to me, instead of puttering around the house, trying to deal with telecommuting and children, and looking at the neverending pile of dishes. I don’t know that I really heard and understood everything I was told after my diagnosis, and it would have helped to have had his (and my) full attention. How do you internalize a possible cancer diagnosis with the sound of your neighbor’s leaf blower in the background? A phone call does not have the gravity of an office visit. Had I received my news in a clinic, I could have gone home to a place that feels safe and secure. Now, I look at the place I was sitting in my living room and wonder if I’m still riddled with cancer. I look at the place I cried with Strange when it sunk in for him that I might still have another battle to face at a young age and that I could die young. It doesn’t feel safe any more. At the very least, I have the recovery from a hysterectomy to deal with. I didn’t have a moment to compose myself before going home. I was already home. Getting my news by phone means that the person delivering it could give me no printed information. She told me to expect my test results in the mail in 7-10 days, which include the data about my individual risk. I realized after that I could remember only a fraction of what she said and kicked myself for not taking more notes. Strange did what he does best. He went to the scientific literature and bombarded us with data about how serious my mutation is. Partially to provide factual information. Also partially to convince himself that his wife isn’t going to die young.
Getting bad news by phone in times of COVID adds additional levels of stress and anxiety. The person who delivered my news asked if I wanted a referral to a gastroenterologist to start screening my lower GI tract and a gynecologist to start screening and discussing my hysterectomy. I can’t even type that without my eyes welling up. Of course, I did. But, because we’re in the middle of a pandemic, it’s entirely unknown when I can schedule a follow-up appointment because non-essential appointments are on hold. I know with every ounce of my rational self that this is alright. I will be fine for a few months while other people that have pressing issues are cared for. That doesn’t stop the irrational part of me from waking up every night at 2 am, putting my hand on my abdomen, and trying to see if I can feel more cancer growing. I’m trying to pretend that everything is normal at work, trying to homeschool the iTots, and trying not to wake up screaming in the middle of the night because I don’t know if the cancer is gone or when it’s coming back. Not if it’s coming back. I’m reading page after page of posts from women who have had complete hysterectomies and wondering in the deepest, darkest parts of the night if my husband will love me less afterward. I don’t want stories of sisterly solidarity. I want to know what cancer risk I’m trading for the early cardiovascular risk that comes from premature menopause.
I grew children there and now my uterus is the enemy.
I’m evolving toward feeling completely numb. If this had been normal times, I would have gone and had a glass of wine with my friend. I would have gone to see my father or my other family. My aunt would have hugged me and made me laugh. I am stuck in the house where I learned that my DNA is my enemy and I have none of my usual coping mechanisms and no information about when I can expect to follow-up with anyone. I thought about calling my primary care doc, who is likely dealing with an avalanche of COVID-possible patients, for help with the anxiety at night. I thought about taking a few days away from work, but it’s hard to see that as a possibility when we’re all being brave soldiers and keeping the lights on for our students. None of it really feels feasible or possible
I know that I needed to know. I just know that I didn’t need to know right now.



Oh Isis, I am so very sorry that you are experiencing this. :(
My nitric oxide bacteria might be able to help. Email me at my company, [email protected]
take care.
Dave
How frightening, and what a horrible time for this to happen. I am so sorry. If there is anything that you need– materially, or just to rant– don’t hesitate to contact me (easiest way is via twitter @biblioteq_tress). I work at a university library, and might have access to a journal or pub you don’t. Also, I live in Boston, & while sheltering-in-place limits some of what I could do, please let me know if you need or want anything from here (including lobster or really good IPA, if either are your thing!). I have friends who work in the Tufts & Harvard medical libraries, & my partner worked at Beth Israel until recently. Info, phone numbers, whatever else, just asked. All the hugs–bibliotequetress